Medical Aid in Dying: ‘They can make the choice that they want’
Published 3:15 pm Friday, May 10, 2024

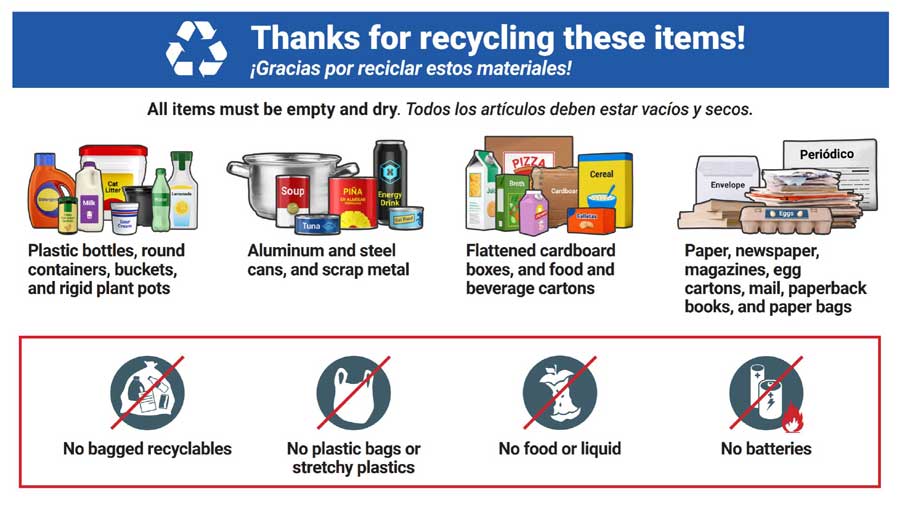
- Jan Rowe holds a photograph of her late husband, Jack, at her home in Medford. The photograph was taken just before her husband's death by medical aid in dying.
It was a Friday before a weeklong vacation, and Jan Rowe of Medford had three dying people on her mind.
Rowe is a local volunteer with the nonprofit End of Life Choices Oregon, an organization that helps walk people with terminal illnesses through options that include Oregon’s Death with Dignity law.
But on that day before vacation only one obtained — and would obtain — the prescription from a doctor for lethal medication.
As Rowe prepared for other volunteers to cover her clients’ needs for the week ahead, she said one client was unable to finish the process in time and instead chose to voluntarily stop eating and drinking.
A third was declining rapidly on their own.
This late April snapshot illustrates the complexities that persist more than two and a half decades after Oregon voters passed the country’s first Death with Dignity law.
The practice of a terminal patient taking a lethal medication prescribed by their doctor requires authorization from two doctors, a typical 15-day wait between the first and second opinion, and rigid requirements related to the patient’s ability to make their own decision and administer their own medication.
As End of Life Choices Oregon volunteers walk beside declining terminal patients they call “clients,” it can be common for nature to take its course.
“You just have to wait to see what the situation is,” Rowe said. “It can be a very minimal process or a very long, drawn-out process.”
Southern Oregon’s growth in the number of terminally ill people who died using Oregon’s Death with Dignity law outpaced the statewide growth rate in 2023. A record 367 Oregon patients died using medical aid in dying in 2023, an increase of 20.7% from the year before. Southern Oregon — across Jackson, Josephine, Klamath, Coos, Curry, Douglas and Lake counties — saw an increase of 30% from the year before. Jackson County alone saw an increase of 22.2%.
Rowe has seen that growth firsthand, and she sat with the Rogue Valley Times at length to discuss her work with End of Life Choices Oregon and walking beside terminally ill hospice patients along their end-of-life journeys, in many cases to their final steps.
“The numbers have increased over the years, and we expect them to increase,” Rowe said.
She attributed the growth to a rise in awareness and a reduction of stigma in the past two and a half decades.
“It means that a greater number of people are not suffering needlessly,” Rowe said. “It means that they can make the choice that they want.”
Asked how statistically significant Jackson County’s increase is, Rowe said it’s grown “in very small steps” since voters passed the law for what was then known as “physician-assisted suicide.” That term is no longer used among hospice workers and caregivers, instead referring to the practice of a patient self-administering doctor-prescribed medication to end their life as “death with dignity” or, more recently, “medical aid in dying.”
In all cases, the organization takes only an assisting role, helping clients access necessary forms and resources for obtaining a lethal prescription, or being present at planned deaths when requested. Rowe said the organization leaves it to the patient at every step. A core tenant of Oregon’s Death with Dignity law is that each patient must be capable of making their own decision and administering the doctor-prescribed lethal medication themself.
“We’re just giving advice and support, but we’re not involved in medical interventions,” Rowe said.
A pro bono doctor’s perspective
Some 167 physicians wrote lethal prescriptions in 2023, including 26 in Southern Oregon, according to the Oregon Health Authority’s annual report. Dr. Bill Southworth of Ashland was one of them.
Southworth is an “active emeritus” physician, meaning that he is semi-retired, and retains his license solely for pro bono work. He has been a consulting physician in medical aid in dying cases for hospice patients since 2016, affirming other doctors’ terminal diagnoses and lethal prescriptions. He has been writing lethal prescriptions since 2018.
“It’s not a trivial decision,” Southworth said.
When he worked in internal medicine, he would commonly do house calls. “Now that’s all I do,” Southworth said. His patients are often declining at their home, and the last thing they want is to visit a doctor’s office.
The law since 1998 has required a 15-day waiting period between requests from their attending physician and consulting physician, but a waiver has been available since 2020 for patients declining rapidly.
“I can’t tell you how many people died waiting … making a request in 15 days,” Southworth said.
He estimates that roughly 28% of the lethal prescriptions he wrote last year were exempted from the waiting period. Southworth says he logs his exemptions, but he’s never been asked.
“But I’m ready if they do,” Southworth said.
Rowe said the wait times were incorporated into the law as a safeguard, but in her experience they are “just a burden” for people who already know they are going to decline.
“A lot can happen in two weeks time,” Rowe said.
Jackson County’s medically aided deaths have grown from 11 in 2018 to 22 in 2023, although the high-water mark thus far was 23 deaths in 2020, according to the Oregon Health Authority. Southworth in an opinion piece attributed the growth of medical aid in dying over the past five years to factors on the patient and physician sides.
The statewide and county numbers make up a fraction of a percent of the statewide and Jackson County deaths. Jackson County’s 22 and Oregon’s 367 medically aided deaths each make up roughly 0.8% of the 2,694 deaths locally and 42,284 deaths statewide.
He said patients are more aware of the option, they no longer feel as ostracized or rejected by their providers when they bring up the subject, and when they do bring it up, doctors and social workers more routinely refer them to organizations like End of Life Choices Oregon to counsel and guide them.
On the physician side, telehealth now helps with medical consultations for patients unable to leave home, and physicians no longer fear being stigmatized.
Southworth is not directly affiliated with End of Life Choices Oregon, but his role as a volunteer physician who specializes in medical aid in dying makes him one the organization commonly calls. No doctor is required to give a prescription under Oregon’s Death with Dignity law, so often when a patient’s primary doctor declines to participate, social workers and volunteers at the nonprofit will reach out to Southworth to step in.
“For many years Bill has been our only pro bono,” Rowe said, adding that their list of doctors is not something they give out.
At 83, Southworth said this year may be his last. His DEA registration as a prescribing physician expires on his 84th birthday and Southworth is reluctant to go through the expense of renewing it.
“I think enough physicians are available to pick up that slack,” Southworth said.
He has recruited two physicians to take his place: one who is fully licensed and works full time, and another who is a retired emergency room doctor who only does the consultation.
End of Life Choices Oregon’s role
The organization’s involvement with a client often begins with a phone call to the organization’s main line, but in some cases End of Life Choices works with doctors.
An intake specialist based in Portland asks if the client has a terminal diagnosis, then takes their information and enters it in a secure database. Based on the client’s location, the specialist will route the case to one of five teams: Southern Oregon, Portland, Salem, Eugene or Bend.
“All of the hospices refer patients to us if their patients ask about medical aid in dying,” Rowe said.
The organization then connects the client with a volunteer to help guide them through the process, including legal requirements, help obtaining a prescription if the client’s doctor declines to participate, and guidance on how to get a waiver in instances where a patient is declining rapidly to the point they fear they won’t be able to self-administer their medication as their terminal condition progresses.
“We tailor our services to you and your family, according to your preferences during this difficult transition,” states an End of Life Choices Oregon pamphlet Rowe provided.
Under Oregon law, to qualify for a Death with Dignity Act prescription, a patient must have a six-month prognosis confirmed by two physicians, they must be 18 or older, they must have the mental capability to make their own decisions and they must be present in Oregon.
Rowe said that she has been seeing clients personally since 2016 and has attended “about a dozen” planned deaths, and she has never seen a case of coercion.
“When you talk with clients who have a terminal diagnosis, they pretty much know what they want,” Rowe said.
In situations where the client wants volunteers present at their planned death, End of Life Choices volunteers typically arrive in pairs. She said the events that culminate with a client consuming their medication can be emotionally charged. Having two volunteers allows one to step in if, say, a family member raises objections.
“You kind of have to tread lightly, and suggest the family member who’s opposed maybe just not be in the room when the client drinks the medication,” Rowe said. “There’s good reason to have two volunteers.”
Rowe estimates that “about a third” of the clients who obtain a lethal prescription never end up using it.
Statewide, the Oregon Health Authority said 560 people had prescriptions written in 2023, and 337 ingested medication that year. Another 30 patients died in 2023 after ingesting prescriptions obtained in a prior year. Another 82 ultimately died from other causes.
The status of another 141 patients who had prescriptions was unknown, as of the latest report, including whether 41 patients who died used their medication.
Rowe said that sometimes a terminal client’s decision not to use their lethal medication is a conscious one, in that the dying process is not as painful or existentially painful as they expect, and the client proceeds to die naturally.
In other cases, the client may have their prescription and plan to use it, but one day their disease takes over. For instance, a patient may have a stroke, “and they literally cannot proceed because they become incapacitated.”
The Southern Oregon team’s territory spans as far east as Lakeview, as far west as the south coast and as far north as Canyonville. The Eugene team typically handles Roseburg cases because those clients’ doctors are usually based in Lane County.
Rowe said Southern Oregon’s volunteer base has grown this year to 14 people. Last year she estimated they “only had about eight or nine.” There are roughly 100 volunteers across the state.
Each new volunteer’s reason for helping is different. For some it may have been that they knew someone in hospice, in others it may have been “a really bad death with a family member” that motivates them to help a client not suffer.
“We might have had an experience with a family member of theirs and that tweaks them,” Rowe said.
Rowe’s story of medical aid in dying
Rowe estimates she has helped more than 75 people in some capacity over the past eight years — whether it was guiding a patient through the forms or just fielding a phone call routed through the call center.
For Rowe, it began with her husband Jack’s medically assisted death in 2014 — and a desire to give others a similar peace.
Before Jack’s terminal blood cancer diagnosis, Rowe said she and her husband hardly ever gave medical aid in dying any thought.
“We knew there was a law here — we didn’t ever necessarily expect to make use of it,” Rowe said.
Jack, a retired neurologist, was too old for a bone marrow transplant. Their oncologist told him chemotherapy may only give him another month. He went on hospice.
“So he just said no. He didn’t want to do chemo, he didn’t want to do anything,” Rowe said.
Rowe said Jack downloaded all the forms and did the paperwork himself. He wanted to set a date right away, she remembered. “But honestly I wasn’t ready.”
“He had so many things wrong with him, we always knew he was going to die before me,” Rowe said. “But just to realize all of a sudden that it was a reality and he was going to die is a different story.”
Jack died on Nov. 11, 2014, at the age of 73. A piece he wrote about his decision ran posthumously in the Sept. 1, 2015, Journal of the American Medical Association.
“Sometimes, for a dying patient, the option of an easy, assisted death is the most merciful, caring, and, I believe, ethical way to do that,” Dr. Rowe wrote. “I personally also believe that if a person knows he is dying, he should not be forced to wait until the unpleasantness actually begins.”